Cell-based therapies and gene-independent approaches have the potential to benefit anyone with Usher syndrome, regardless of their subtype. Examples include stem cells, retinal progenitor cells, neuroprotection, optogenetics, nutritional approaches, etc. Here, we outline the various approaches that have the potential to help anyone living with Usher syndrome.
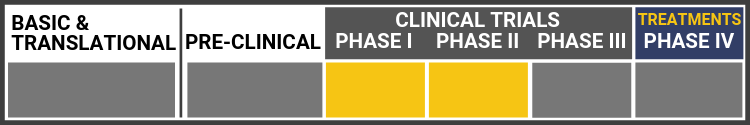
Each research project listed below will include a graphic of the research continuum. The gold box indicates where this project falls on the continuum, illustrating its progress towards reaching people living with Usher syndrome, from "Bench to Bedside."
Click here to learn more about the different stages in the research continuum.
Safety and Efficacy of NPI-001 Tablets for RP Associated With Usher Syndrome (SLO RP)

Dr. Lee Anderson with sponsors and collaborators from Nacuity Pharmaceuticals Inc. and Foundation Fighting Blindness in Australia are looking at NPI-001 Tablets, an antioxidant drug. Their study will examine the safety and efficacy of these oral NPI-001 Tablets compared to placebo tablets for participants who have vision loss due to retinitis pigmentosa (RP) with Usher syndrome. The study takes place over the course of 24 months. This study is expected to be completed in September 2023.
Nacuity Pharmaceuticals Info Page
Link to study details on ClinicalTrials.gov
Stem Cell Therapy for USH


Edwin Stone, M.D., Ph.D.:
University of Iowa
Stone and his team at the University of Iowa are working to develop a cure for Usher syndrome along with other types of retinitis pigmentosa. They are working to halt further retinal degeneration from USH1F through gene replacement and to repair damaged retinal photoreceptor cells with new cells made from the patient's own skin cells with the goal of a clinical trial once safety and efficacy are determined.
The University of Iowa Institute for Vision Research
ReNeuron

Clinical Trial for Safety and Tolerability of hRPC in Retinitis Pigmentosa (hRPCRP)
ReNeuron, a UK-based stem cell research company, that focuses on developing stem-cell therapies that target areas of "significant unmet or poorly met medical need." They have used their stem cell technologies to develop cell-based therapies for significant diseases where cells can be readily administered to any eligible patient without the need for additional drug treatment. Currently, they are developing the human retinal progenitor cell line (hRPC) for the treatment of retinal diseases such as retinitis pigmentosa (RP).
- Positive Preliminary Data: Significant improvement in vision in first cohort of Phase II subjects in US trial of hRPC cell therapy in retinitis pigmentosa (February 20, 2019)
- ReNeuron Website
- Additional Information on hRPCs for Retinal Diseases
- Clinical Trial for the Safety and Tolerability of hRPC in Retinitis Pigmentosa (hRPCRP)
jCyte

Clinical Trial for Safety and Efficacy of Intravitreal Injection of Human Retinal Progenitor Cells in Adults With Retinitis Pigmentosa
jCyte was founded in 2012 by Drs. Henry Klassen and Jing Yang, who have spent decades investigating the mechanisms that drive retinitis pigmentosa (RP) and other retinal diseases. Their work led to the creation of retinal progenitor cells (RPCs), a type of stem cell that can only become retinal cells. Clinical studies have shown that these cells could rescue and even replace diseased retinal cells. Early results from a phase 1/2a study have shown the treatment is safe and does not trigger an immune response. They have completed the enrollment and recruitment for their current phase 2b trial.
- jCyte Website
- Additional Information on jCells
- ClinicalTrials.gov listing for Phase 1/2a Study
- ClinicalTrials.gov listing for Phase 2b Study
Cedars-Sinai

Cedars-Sinai
Cedars-Sinai, a non-profit healthcare organization based in Los Angeles, has received authorizations from the FDA to launch a 16-person, Phase 1/2a clinical trial of human neural progenitor cells--stem cells that have almost developed into neural cells--for patients with RP. The trial is being funded by a $10.5 million grant from the California Institute for Regenerative Medicine. The study's principal investigator is Clive Svendsen, PhD, professor of Biomedical Sciences and Medicine and director of the Cedars-Sinai Board of Governors Regenerative Medicine Institute.
Gene-Independent Approaches: Related Science News
Cell therapy, a cutting-edge therapeutic approach, involves transplanting healthy human cells to replace or repair diseased or damaged cells, thereby restoring function.
Many modalities are being evaluated for the treatment of retinal degenerative diseases such as retinitis pigmentosa (RP), including stem cell therapy where dead or damaged cells are replaced by healthy ones.
In the summer of 2022, Endogena launched its first phase 1/2a study of EA-2353 for retinitis pigmentosa (RP).
In the summer of 2022, Endogena launched its first dosing of its phase 1/2a study of EA-2353 in retinitis pigmentosa (RP).
Researchers at the University of Wisconsin-Madison have been working with stem cells to grow organoids in a petri dish that resemble the retina.
Researchers used stem cells from an individual with retinitis pigmentosa (RP) caused by mutations in their USH2A gene to create retinal organoids (ROs), that mimics the retina to be used as an in vitro RP disease model.
Research is being conducted at the University of Pennsylvania School of Veterinary Medicine, with the University of Wisconsin, Children's Hospital of Philadelphia and the National Institutes of Health’s National Eye Institute for a cell therapy for people with retinal disorders.
A team of researchers from Germany's Center for Regenerative Therapies Dresden (CRTD) reported positive results in their pre-clinical studies where lab-grown human photoreceptor cells (cones) were transplanted into mice with damaged cones.
At the University of Wisconsin-Madison, researchers are studying stem cells and how they could potentially treat retinal diseases, including retinitis pigmentosa and Usher syndrome.
In a guest column at clinicalleader.com, the authors discuss the past and exciting future prospects of optogenetic therapies.
Researchers at the University of Wisconsin School of Medicine and Public Health were able to create retinal cells from human stem cells that can detect light and change it to electrical waves.
Researchers in China successfully created an induced-pluripotent stem (iPS) cell line using immune cells from the blood of a patient with Usher syndrome type 2A.
Researchers at Newcastle University are looking into creating treatments for common inherited eye conditions.
A recent biotechnology breakthrough is the organ-on-chip (OOC) technology.
AIVITA Biomedical Inc., a biotech company that specializes in new ways of using stem cells, recently conducted a preclinical study. Using human stem cells that they created, researchers created and tested a “total retina patch” for vision loss.
GenSight Biologics is a biopharmaceutical company that focuses on creating gene therapies for retinal neurodegenerative and central nervous system disorders. They have announced that the FDA has awarded Fast Track Designation of GS030, which uses AAV2 gene therapy combined with optogenetics to treat retinitis pigmentosa.
Researchers have been exploring stem cell therapies to treat vision loss, including vision loss caused by retinitis pigmentosa. Preclinical and clinical studies are showing that stem cell therapies could be new options.
A Phase 2 clinical trial was used to see if injecting human retinal progenitor cells (derived from stem cells) can improve vision and visual fields in people with retinitis pigmentosa (RP).
Nanoscope Therapeutics Inc., a clinical-stage biotechnology company, has recently announced that one of its drugs is approved for Phase 2b clinical trial.
Retinitis pigmentosa (RP) is a rare genetic disease that causes loss of photoreceptors, which are the light sensitive cells in the retina. This disease can lead to blindness and affects more than 2 million people worldwide. In a groundbreaking clinical trial led by Paris-based GenSight Biologics, a man who was blind for 40 years successfully regained some visual function with a technique called optogenetics. Optogenetics uses light to control neuron activity. In this study, a light-sensing protein called ChrimsonR was injected into the eye and delivered to the patient’s retinal cells. After a four-month period to allow his body to make ChrimsonR protein, the patient was fitted with special goggles that detect and shift incoming light into a specific color range. The patient was able to see high-contrast images and objects, and his brain activity was the same as someone with normal sight.
What this means for Usher syndrome:
More patients will need to be enrolled and evaluated, but if this study proves to be successful, RP patients who are blind may be able to regain some sight, increasing their quality of life. Because vision loss in Usher syndrome is a type of RP, this therapy may also be beneficial for Usher syndrome patients.
Individuals that have permanent damage to their photoreceptors are unable to repair or regenerate new photoreceptors. Researchers and engineers may have a possible solution for these individuals living with vision loss. They have worked to make new photoreceptors and a micro-molded scaffolding photoreceptor “patch.”
Magdalene Seiler, Ph.D., UCI associate professor has been awarded a five-year grant of $3,823,950 from the National Institutes of Health to do a preclinical study using rodent models. This study looks at an innovative co-graft method to permanently repair damaged retinas.
Photoreceptor precursor cells that were generated from stem cells were able to be successfully transplanted into the retina and demonstrate basic visual function.
In a recent study, retinal cells coming from adult human eye stem cells were successfully put into the eyes of monkeys.
An interdisciplinary team of scientists funded by University of Toronto’s Medicine by Design initiative believes they can improve the outcomes of conditions like age-related macular degeneration and retinitis pigmentosa.